Nutrition Counseling for Patients with Prediabetes or Diabetes
More than 86 million Americans over the age of 20 have prediabetes, 29 million Americans are diagnosed with diabetes, and another 8.1 million Americans are living with undiagnosed diabetes.
Diabetes statistics are alarming. More than 86 million Americans over the age of 20 have prediabetes, 29 million Americans are diagnosed with diabetes, and another 8.1 million Americans are living with undiagnosed diabetes. Diabetes remains the seventh leading cause of death in the United States. Complications and comorbid conditions such as hypertension, dyslipidemia, stroke, blindness, kidney disease, and amputations negatively impact quality of life and health care costs.1
Patients with chronic diseases often ask their health care providers what they should be eating or say they know they are eating foods they shouldn’t be eating. They ask their provider to validate what they are hearing about diet, such as “Don’t eat anything white, don’t eat fruit, only eat sugar-free, don’t eat carbs, and don’t eat high fructose corn syrup.” Lately, they have been asking questions about avoiding artificial sweeteners.
Because diabetes is a progressive disease, it is important to help patients recognize the condition’s risk factors and take preventive action. Being overweight or obese is a leading risk factor for type 2 diabetes (T2D). Both can result in insulin resistance and are risk factors for hypertension. The Diabetes Prevention Program (DPP), a major federally-funded study of 3234 individuals at high risk for diabetes, showed that moderate diet and exercise for about 30 minutes or more 5 or more days per week, or for 150 or more minutes per week, resulted in a 5% to 7% weight loss that can delay and possibly prevent T2D.2Health care providers sometimes miss the opportunity to raise their patients’ awareness and help them improve their insulin sensitivity, warning them only to “watch the sugars.”
The dietary recommendations for individuals with prediabetes and T2D are similar to the 2015 Dietary Guidelines for Americans and are often considered “the way everyone should eat.” It all starts with consuming a diet based on the guidelines at ChooseMyPlate.gov. The 2013 nutrition therapy recommendations for the management of adults with diabetes from the American Diabetes Association emphasizes an eating plan that includes a variety of personally and culturally specific food choices in the appropriate amounts of quality carbohydrates, proteins, and fats, individualized to accommodate a patient’s energy needs, food preferences, and medications. Recommendations for fiber and sodium are the same as for the general public.3
Nutrition therapy is recommended for all patients with type 1 diabetes and T2D as an effective component of the overall treatment plan.4Individuals with diabetes should receive individualized medical nutrition therapy (MNT), as needed, to achieve treatment goals, preferably provided by a registered dietitian nutritionist (RDN). Research indicates that MNT can reduce glycated hemoglobin levels from 0.5% to 2% and has its greatest impact when made available to patients when diabetes is first diagnosed.3Unfortunately, only a small percentage of patients with diabetes are referred to an RDN, mostly because many health plans do not include MNT as a covered benefit.
The specific goals of MNT are to:
1. Attain individualized glycemic, blood pressure, and lipid goals;
2. Achieve and maintain body weight goals;
3. Delay or prevent the complications of diabetes;
4. Maintain the pleasure of eating by providing positive messages about food choices; and
5. Provide patients with practical tools for day-to-day meal planning rather than focusing on individual nutrients.
Modest weight loss can be achieved through intensive lifestyle interventions, such as counseling about nutrition, physical activity, and behavior change with ongoing support. If weight loss cannot be achieved, the goals should turn to the prevention of weight gain. Self-monitoring of blood glucose, weight, and food intake has been shown to be effective for both weight-loss and weight-gain prevention.
Specific Macronutrient Considerations
Carbohydrates
Carbohydrate intake has a direct effect on postprandial glucose levels in patients with diabetes and is the primary macronutrient of concern in glycemic management. Ideally, patients should choose nutrient-dense, high-fiber carbohydrates such as vegetables, fruits, legumes, and whole grain breads and cereals throughout the day. Consuming sugar versus starch of the same caloric value may have similar blood glucose effects; however, health care providers should advise minimizing added sugar to nutrient-dense food choices. The nutrition therapy recommendations suggest avoiding sugar-sweetened beverages to reduce the risk for weight gain and worsening of other cardiometabolic risk factors.
Because fiber is not absorbed, it also was once suggested that the grams of fiber be subtracted from the total grams of carbohydrates in a food; however, guidelines for glucose management no longer support this practice. Insufficient evidence exists to support a specific amount or percentage of calories from carbohydrates for patients with diabetes. For patients who monitor grams of carbohydrate, 45 to 60 g of carbohydrates per meal is recommended. For individuals focusing on serving sizes, 3 to 4 servings of a carbohydrate are recommended per meal.
Substituting low—glycemic-load foods for high–glycemic-load foods may modestly improve glycemic control, but does not have strong support in the literature. The inclusion of proteins or fats with carbohydrates may lower the glycemic index.
Protein
For patients with T2D, protein increases insulin response without increasing plasma glucose concentrations. There is no ideal amount of protein intake for optimal glycemic control, so it should be individualized. Proteins consumed with carbohydrates at intervals throughout the day can improve insulin response, resulting in a lowered postprandial glucose response. However, because of protein’s effect on insulin response, proteins should not be consumed with carbohydrates during a hypoglycemic episode. Consistent with the Dietary Guidelines for Americans, patients should always select lean proteins.
Fat
Study results suggest that a Mediterranean-style diet, rich in monounsaturated fats such as walnuts and olive oil, may benefit glycemic control and cardiovascular disease risk. According to the Evidence Analysis Library of the Academy of Nutrition and Dietetics, a 5% energy replacement of saturated fatty acids with monounsaturated fatty acids improves insulin responsiveness in insulin-resistant and patients with T2D.5Limited evidence suggests that omega-6 polyunsaturated fatty acids have this same impact. Research does not support supplementation with omega-3 supplements, yet it is still recommended that patients with diabetes consume a diet rich in long-chain omega-3 fatty acids because of their beneficial effect on lipoproteins. Saturated fat intake should be limited consistent with the recommendations for the general population.
Practical Tips and Considerations
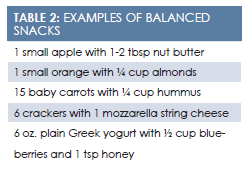
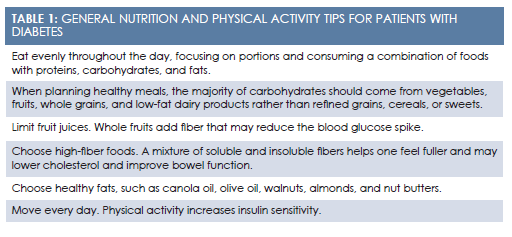
Nutrition counseling is both an art and a science. Information on what to eat (Table 1andTable 2) is based on science, while helping patients make changes in their diet behavior is an art. When talking with patients about their diet, the approach and the conversation can greatly affect engagement and compliance. Traditional nutrition counseling consists of the following steps:
- Explain why the patient should make a change.
- Detail the benefits of making the change.
- Inform the patients how to make the change.
- Emphasize the importance of making the change.
- Tell the individual to do it.
Weight loss has been shown to delay and possibly prevent diabetes. When you lose weight, you are going to feel so much better and your glucose, and likely your lipids and blood pressure, will go down. One suggestion I can give you is to start by cutting your portions in half. It is really important that you do this so you will live to see those grandchildren grow up. So, what do you say that you give this a try?
For example, to help a patient lose weight, a provider might say:
Recently, study results have validated the use of motivational interviewing (MI) as a more effective style of communicating and method of interacting with patients.6Rather than telling the patient what to do, MI identifies and mobilizes the individual’s desire for change within an atmosphere of compassion and acceptance. To gain comfort with an MI style, think about its similarities with shared decision making. Just as with shared decision making, MI is a collaborative process that engages patients, taking into account their values and preferences. It provides options for empowering the patient as an active member of his or her care so that the patient feels heard.
Key communications skills in MI include asking open-ended questions, affirming, reflecting, summarizing what the patient has said, and then—and only then—providing information and advice with the permission of the patient. The goal is to listen for words the patient says that indicate a desire, ability, reason, or need to change—as opposed to a provider projecting these ideas to the patient. When a patient says out loud his or her reason for change, it increases the likelihood of change.
Case Study
Mr. Jones sees his health care provider for upper respiratory symptoms. His body mass index is 28 and his blood pressure is 125/85 mm Hg. He states he was just diagnosed with diabetes. The provider asks Mr. Jones what he knows about diabetes. He replies, “I know I should lose some weight,” and asks if there is any diet he can follow.
The providor could easily have given Mr. Jones a quick answer, but instead he asks, “Have you tried losing weight in the past?” Mr. Jones says he has tried everything. The provider asks if any diet was more successful, and Mr. Jones answers that he had the best luck when he saw a dietitian who helped him plan meals and snacks to go with his crazy schedule. It was when he stopped the dietician visits that he started gaining back the weight.
The provider continues to document Mr. Jones’ upper respiratory symptoms, as Mr. Jones states that he seems to be sick more often now that he has diabetes. The provider asks if he understands why and if he would mind hearing how the body changes with diabetes. Mr. Jones agrees to listen and when asked what he makes of the information, he says, “I really never knew this. I can’t be sick this much because I have to be on the road a lot for work, and I have to concentrate a lot, which I can’t do when I’m sick.” The provider responds:
From what I hear you say, you don’t like to feel poorly and some of your recurrent illnesses may be because your blood sugar isn’t where it should be. You recognize that weight loss is really important to help keep your blood sugar under control, and you have a crazy schedule that doesn’t make following a diet easy to do. You had the best luck when you saw a dietitian, but after you stopped those visits, life got back in the way, and you gradually went back to your old ways of eating. Did I miss anything?
Mr. Jones nods and reiterates that he needs to feel good for his job. He also says he works long days and notices his energy gets low and his concentration gets bad when he goes too long without eating. After asking and receiving the patient’s permission to give some advice, the provider then says, “I can pull out a diet plan to give you or I can direct you to a website, but from what you just said about your lifestyle, a dietitian was helpful to you once and can be helpful for you again. What are your thoughts about going back to see a dietitian?”
Mr. Jones replies that it might be his best bet, but he needs a referral and needs to see one with flexible hours. The provider offers to help investigate dietitians near his home or work that have evening and weekend hours and then asks permission to share one more thing that may help Mr. Jones feel better and have better blood sugar control with his long days. With permission, the provider shares a handout that lists easy, balanced snack ideas, and Mr. Jones gladly takes it.
Before Mr. Jones leaves, the provider asks, “Besides a prescription, how have I helped you today?” Mr. Jones smiles and says, “You’ve helped me realize that I didn’t need another piece of paper, but instead needed a personalized approach to lose weight and get my diabetes under better control.” He also appreciates the snack handout and says he was happy he wasn’t judged for being overweight.
In this scenario, 2-way communication, not lecturing, was the method of dialogue used with the patient. Mr. Jones felt that the provider cared and he felt listened to. It was more important that the provider refer him to a dietitian rather than hand him information. Other patients may ask for specific tools, such as a better understanding of which foods contain carbohydrates. With just a few open-ended questions and reflections to confirm understanding patients’ needs and motivations, these encounters can be more engaging and patients will likely better receive and use the information providers give them.
Summary
No single meal plan or eating pattern works for everyone with diabetes. MNT should be individualized for each patient based on his or her health goals, culture, and health literacy. Portion control and balance of nutrients consumed in regular intervals is the basis of glucose control. Behavioral changes take time, so a collaborative, nonjudgmental approach increases the likelihood of patient’s engagement and compliance. As early as possible, the patient with diabetes should be referred to an RDN who has in-depth knowledge of food and nutrition to help develop an individualized meal plan.
Eileen is currently the vice president of retail dietetics & nutrition solutions for The Little Clinic, responsible for strategy and successful execution of nutrition services in the clinics and stores. Prior to this role, Eileen was VP, Affiliations and Patient Centered Strategies, for The Little Clinic, responsible for creating and developing clinical partnerships across the health care industry. She received her BS in nutrition from the Pennsylvania State University and her master’s in public health from the University of North Carolina. She has received numerous “Excellence in Practice” awards within the nutrition and dietetics profession. She also published a book by Helm Publishing,Winning the War Within: Nutrition Therapy for Clients with Eating Disorders,a teaching manual for clinicians working in the field of eating disorders.
References
- Statistics about diabetes. American Diabetes Association website. diabetes.org/diabetes-basics/statistics/. Updated April 1, 2016. Accessed August 23, 2016.
- Knowler WC, Barrett-Connor E, Fowler SE, et al; The Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin.N Engl J Med.2002;346(6):393-403.
- Evert AB, Boucher JL, Cypress M, et al. Nutrition therapy recommendations for the management of adults with diabetes.Diabetes Care.2013;36(11):3821-3842. doi: 10.2337/dc13-2042.
- Franz MJ, Powers MA, Leontos C, et al. The evidence for medical nutrition therapy for type 1 and type 2 diabetes in adults.J Am Diet Assoc.2010;110(12):1852-1889. doi: 10.1016/j.jada.2010.09.014.
- DLM: major fat components 2011. Academy of Nutrition and Dietetics Evidence Analysis Library website. andeal.org/template.cfm?template=guide_summary&key=2984#supportevidence,2011. Accessed August 23, 2016.
- Rolnick S, Miller WR, Butler CC. Motivational interviewing in health care: helping clients change behavior. New York, NY: Guilford Press: 2008.