Mitigating Malpractice Risks in Retail Care
Being proactive rather than reactive can go a long way toward leading to optimal outcomes in clinical practice.
As the saying goes, the best defense is a good offense, or to put it another way, being proactive rather than reactive can go a long way toward leading to optimal outcomes in clinical practice. Because the retail health model is one of the newer concepts in care delivery, patient expectations may not always be realistic. One thing we as providers never want to consider is the potential for being sued. Knowledge is power, and understanding the standards to which we are held is critical in providing high-quality patient care. In the retail setting, we should follow the same quality practice standards as in any other area of medicine. Adhering to sound clinical guidelines can help mitigate malpractice risk. The following are some basic guiding principles for clinical practice in retail clinics that will help minimize the risk of malpractice actions.
Off-Label Prescribing
This is perhaps one of the easiest traps to fall into. Not knowing the intended use of the medications you prescribe can have serious consequences. Whether prescribing a medication for a newly diagnosed condition or providing a medication refill to a patient, be sure the condition for which it is being prescribed aligns with its indication and use. Some states limit the ability of providers to prescribe off-label medications or treatments, whereas other providers may have practice restrictions within their organization. It is important to know what you may and may not order and whether off-label prescribing is permitted. If a patient experiences an adverse effect (AE) as the result of taking a medication outside of its intended use, there could be potential implications beyond litigation. If a contractual practice agreement has been violated, it may lead to challenges if you were to find yourself the subject of a lawsuit and may not have the backing of your organization.
Evidence-Based Guidelines
These play a role in establishing a framework for assessment, documentation, and treatment of conditions. If clinical care is ever called into question, and the documentation illustrates adherence to standard of care, the clinical note will stand on its own merits. A history and physical exam that follows evidence-based guidelines demonstrates the fact that a provider performed the appropriate assessment and ruled out the possibility of more serious conditions. Disease management is the other part of evidence-based guidelines that are too often overlooked. Remember that evidence from validated studies provides the grading for recommendations in the treatment of conditions to determine the most appropriate first-line treatment. Deviating from this is acceptable when clinical criteria warrants, but if there is no evidence to show the clinical decision making and the patient has an AE, the provider would not have the clinical backing they need.
Scope of Practice
State regulations can vary on what licensed providers are allowed to perform, so knowing what your state scope of practice allows under your licensure is important. Providers should exercise caution if considering rendering services that they have not been trained, licensed, or certified to perform. Pair this with being aware of limitations on your malpractice policy, whether an individual policy or coverage provided by your employer. Malpractice policies often contain language that limits coverage to services within the scope of licensure or certification. If you provide services that are outside of this scope, your policy may not protect you if a patient has an AE that results in litigation.
Defensible Documentation
Remember that you cannot defend what you did not document. Attorneys are not alone in espousing that if something is not documented, it makes it very difficult to prove it was done. Your clinical note should reflect accurately the care that was rendered and provide a depiction of the clinical decision making. One area where providers tend to become complacent is with physical-exam findings. Remember that documenting pertinent negative findings is equally important as documenting key positive findings and aligns with standard of care principles and guidelines.
This does not mean that every patient encounter should be cookie cutter. Documentation should be complete for the clinical picture yet concise and individualized. Too much documentation can give the appearance that the provider is unsure of his or her assessment and repetitive documentation can give the appearance that the provider documents the same thing over and over. Either of these could have implications were the documentation to be questioned in a legal proceeding. Remember that in cases of litigation, the clinical note will act like another “witness” in the case. Defensible documentation will leave little room for cross-examination.
Vaccine Administration
Although vaccine administration may seem like a simple task, do not forget all the necessary safeguards to ensure patient safety. Although vaccine errors may rarely cause a serious problem, it only takes one occurrence of a bad outcome to place a provider at risk. The 5 “rights” should be reviewed with every vaccine administration: right patient, right dose, right vaccine/diluent, right route, right time. Two of the most common vaccine administration errors are administering an expired vaccine and giving a vaccine outside of the FDA-approved age requirements.
As providers, we are responsible for any vaccination we administer. Even when a patient presents with an order from a primary care provider, if it is off-label, think twice before following that order. Lastly, remember that a vaccine reaction can occur at any time, but many commonly occur within minutes of administration, and anaphylaxis is most common within the first 5 minutes post-vaccination. Having the patient wait in the clinical area post-vaccination is a simple practice that can help minimize the risk of a serious event should such a reaction occur.
Don’t Underestimate
Remain alert so as not to become overconfident when assessing minor problems, and be alert for subtle red flags. Don’t discount a complaint just because it doesn’t appear to fit the expected differential diagnosis. Sometimes, serious conditions can mask other symptoms. However, don’t be hypervigilant for every patient complaint. Providers should use their critical-thinking skills to connect symptoms or identify signs of more serious conditions. Another important consideration is to not discount the frequent flier. When a patient presents multiple times for the same complaint, and it is a condition that should be better controlled or more responsive to treatment, don’t ignore potential warning signs. Remember to refer when appropriate.
Don’t Fall Short on Follow-Up
Follow-up is almost twice as important in retail care as it may otherwise be in primary care. Remember, many times, we do not have an ongoing relationship with patients in this context to know that they will follow through on the treatment plan or recommendations for follow-up. Providers cannot force a patient to comply with recommendations, but we must demonstrate due diligence to inform the patient about the importance of following through. If they still elect not to adhere to the plan, ownership and accountability for the outcome begins to transfer to the patient.
Definite Diagnosis
ICD-10 diagnosis expansion has given many more options and hence more opportunity for incorrect selection. Be certain of what you are diagnosing, and review your final selections before putting a diagnosis code on the clinical record. As simple as it may sound, patients have sued for incorrect diagnosis codes. Imagine being diagnosed with cancer when you have never had cancer in your life and now that is part of your claim history. Much like a credit report, incorrect information is very difficult to get removed once that claim has been submitted to the billing server and processed.
Conclusion
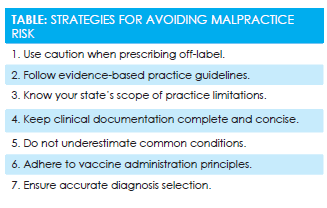
While the fear of litigation may always loom for providers in the medical profession and retail setting, solid practice guidelines and documentation principles can be your best tools to significantly reduce that risk. SeeTablefor a summary of the strategies presented here to help you mitigate malpractice risk.
Dr. Hayes is a board-certified nurse practitioner, coder, and compliance officer with more than 25 years of health care experience. She currently works for Walgreens Healthcare Clinic serving in the capacity of Manager, Medical Coding, and Compliance Liaison.