UTI Treatment at a Retail Clinic
Urinary tract infections in women comprise a significant number of retail clinic visits.
Urinary tract infections (UTIs) in women comprise a significant number of retail clinic visits. Since the presentation of UTIs can often be atypical,1the retail clinician must maintain a high suspicion when considering a variety of symptoms. To highlight the clinical workflow for UTI cases, the following describes a patient who recently presented to a retail clinic.
KD was sitting in the waiting area when the nurse practitioner (NP) arrived at work in the morning before the retail clinic opened. The 38-year-old woman was bent over in the waiting room chair, holding her head and shielding her eyes while gently rocking back and forth. When the NP asked the patient what was going on, the patient replied, “I need something for my migraine.”
DISCUSSION QUESTION:What information will be important to accurately diagnose and treat KD’s current complaints?
ANSWER:Past medical history, migraine history, previous migraine treatments, other medications, and other symptoms will all be important.
Once KD was checked into the clinic’s electronic medical record, it was discovered that she carried a past medical history of migraine headaches and morbid obesity. She denied hypertension, diabetes, cardiovascular disease, and seizures. The only medication she was currently taking was oral birth control pills that had not been changed in 3 years. At an emergency room (ER) visit over a year ago, the patient had been prescribed sumatriptan 50 mg, but she no longer had an active prescription.
KD reported that her migraines started about 3 years earlier, shortly after she delivered her son without complications. Her headaches were generally responsive to immediate administration of ibuprofen 800 mg and rest in a dark room. However, a “couple times a year,” the headaches were severe enough that she needed to take 1 dose of the sumatriptan, as well as promethazine 25 mg. She revealed that she did not tolerate the nasal form of sumatriptan. Triggers had not been identified.
Today’s headache started 6 hours earlier and had developed over about an hour to its current pain level of “9.” KD denied that it was her worst headache ever, but she quickly added that she knew it was not going to go away on its own. She had taken ibuprofen 800 mg about an hour after the headache started with no discernible difference. She denied pregnancy, aura, visual disturbance, and extremity or facial weakness/numbness, but she admitted to photophobia, phonophobia, and nausea. Pain was located mainly in the frontal and right temporal regions and was “throbbing.” Any kind of activity or movement worsened the pain and nausea.
​DISCUSSION QUESTION:With this much focus on the migraine history and symptoms, what are the most important systems to assess during KD’s physical examination?
ANSWER:A thorough neurologic exam would rule out more serious conditions that might warrant imaging and blood work, but the best practice is to always start with the basics: blood pressure, temperature, respiratory rate, and heart rate, as well as auscultation of the heart and lungs.
On physical exam, KD had a blood pressure of 154/94 mm Hg, heart rate of 98 bpm, respiratory rate of 20 breaths/ min, and oral temperature of 101°F. Her last menstrual period was 2 weeks ago. She was still gently rocking in the exam chair holding one hand over her eyes to shield them from the light, but now the other hand was massaging her left flank. Her skin was warm and dry, and there was no temporal tenderness. Her pupils were equal, round, and reactive to light and accommodation, although this assessment was uncomfortable for KD. With the lights off and the door ajar for low light, extraocular muscle movement was found to be grossly normal. A cranial nerve check was otherwise normal, as well. Left costovertebral angle tenderness and suprapubic pain were both solicited on exam.
In the setting of KD’s fever and flank pain, which are unusual symptoms for migraine, the NP requested a urine sample. KD produced a dark, concentrated, cloudy, non-bloody urine specimen, and the urinalysis results revealed large amounts of hemolyzed blood, positive nitrites, and leukocytes.
When questioned further, KD admitted that she had been having urinary frequency, foul-smelling urine, and burning with urination for 1 to 2 days prior to the onset of her headache. She had been very busy with work and caring for her 3-year-old son, and she had not sought any medical help. She did not realize that she was running a fever and she stated that she had a UTI approximately 10 years earlier, yet she did not recognize the symptoms these past few days.
DISCUSSION QUESTION:What would be the differential diagnosis for KD at this point, given her symptoms of migraine with a basically normal neurologic exam, elevated temperature, positive dipstick on urinalysis, and flank pain?
ANSWER:KD did in fact have a migraine, but she also had the triad of fever, nausea, and flank pain, so pyelonephritis has to be included in the differential diagnosis (Table 1).2However, other significant symptoms were missing, including tachycardia, vomiting, chills, and severe flank pain.
TABLE 1: DIFFERENTIAL DIAGNOSIS
Pyelonephritis
Urinary calculi
Diabetes
Urinary malignancy
Interstitial cystitis
Vulvovaginitis
Incontinence
UTI
The NP recommended that KD immediately go to the local ER for suspected pyelonephritis. The NP explained to KD that the migraine she was experiencing could have been triggered by the UTI, and both could be treated at the ER.
DISCUSSION QUESTION:What do you think the treatment plan would be for KD if it was determined that she did not have pyelonephritis?
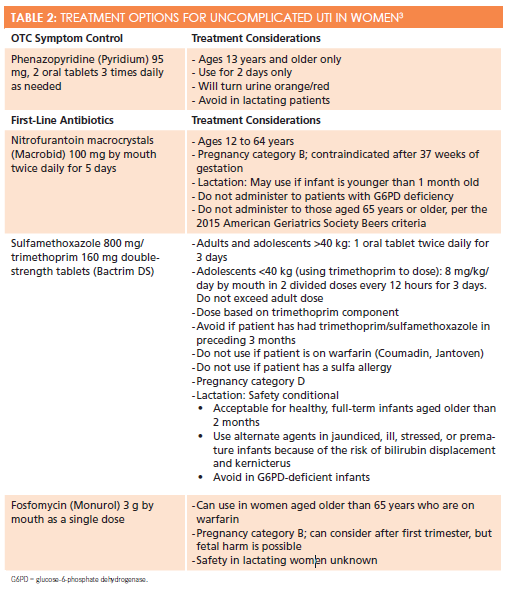
ANSWER:Table 2presents treatment options for uncomplicated UTI in a nonpregnant woman without a recurrent history of UTI.3
Upon follow-up phone call, KD reported that she was seen at the ER and received subcutaneous sumatriptan as well as oxygen when she arrived, and then was discharged with oral ciprofloxacin 500 mg to be taken twice daily for 1 week. She said the ER staff did not think she had a kidney infection, but cautioned her to return immediately if she was not feeling better in 24 hours. Ultimately, KD recovered well on the oral antibiotic regimen.
KD’s case illustrates a challenge that retail clinicians encounter: a significantly symptomatic patient who presents with a request for treatment of what he or she thinks is the underlying cause of symptoms. With or without access to lab work that could show basic leukocyte counts and electrolyte balances, the clinician needs to assess basic past medical history, symptoms, and physical exam clues in detail to determine whether the patient’s “self-diagnosis” is accurate. In this situation, if the provider had capitulated to the patient’s request for sumatriptan and promethazine to treat what she “knew” was simply a migraine, the UTI very likely could have progressed to a more dangerous pyelonephritis, putting the patient at much higher risk for complications and incurring higher overall health care costs.
KD verbally admitted during the visit and on the follow-up call that she had not wanted to go to the ER for her headache and was “waiting it out at home,” hoping that it would subside. Her mother suggested that she go to the retail clinic instead, where the wait time was shorter and the cost was lower. KD agreed, and as a result, she was seen earlier in her infectious process than if she had stayed at home until later in the day or even the next day, when she finally may have realized that she needed to go to the ER.
Retail clinics offer patients a more accessible entry into the health care system and are often seen as a less intimidating gateway to quality care comparable to that of urgent care facilities and ERs. Retail clinicians offer the very necessary service of assessing patients, establishing the level of care that patients need, and educating patients on how to access that care, given that patients with inappropriately high acuity can present to retail clinics.4
Mary Kegelman is a doctorally prepared nurse practitioner. She is a senior practice manager at MinuteClinic working to enhance the professionalism and visibility of nurse practitioners.
References
- Matthews SJ, Lancaster JW. Urinary tract infections in the elderly population.Am J Geriatr Pharmacother. 2011 Oct;9(5):286-309. doi: 10.1016/j.amjopharm.2011.07.002.
- Colgan R, Williams M, Johnson JR. Diagnosis and treatment of acute pyelonephritis in women.Am Fam Physician. 2011;84(5):519-526.
- Gupta K, Hooton TM, Naber KG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases.Clin Infect Dis. 2011;52(5):e103-e120. doi: 10.1093/cid/ciq257.
- Shrank WH, Krumme AA, Tong AY, et al. Quality of care at retail clinics for 3 common conditions.Am J Managed Care. 2014;20(10):794-801.