Incorporating Chronic Care Programs into Convenient Care Clinics
Retail-based convenient care clinics continue to grow and expand their footprint throughout the country.
Retail-based convenient care clinics continue to grow and expand their footprint throughout the country. Today, there are more than 2000 convenient care clinics in 41 states and the District of Columbia, and this number is expected to exceed 2800 by 2017.1These clinics have proven to be popular because they offer consumers easy access to high-quality, affordable health care.
Increasingly, large health care systems are recognizing the value of partnering with convenient care providers to offer quality care at a lower cost through multiple, community-based locations. The care delivered through convenient care clinics costs 30% to 40% less than similar care at physicians’ offices and urgent care centers, and approximately 80% less than similar care at emergency departments.2
The Scope of Chronic Disease
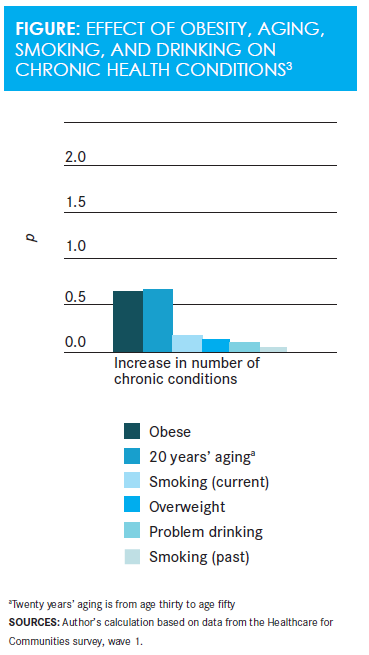
Chronic diseases, such as heart disease and diabetes, are the main drivers of morbidity and mortality in the United States. Aside from genetic makeup, obesity, sedentary lifestyle, and smoking are the major risk factors for developing chronic diseases. Notably, obesity has about the same association with chronic health conditions as 20 years’ aging, and it greatly exceeds the associations of smoking or alcohol abuse (Figure3). An alarming proportion of individuals who are obese have conditions like prehypertension, prediabetes, or metabolic syndrome, which progress over time to diabetes, heart disease, arthritis, and cancer.
The scope of the problem is enormous. In America4:
- Approximately 37% of adults aged 20 years or older have prediabetes
- 31% of adults have prehypertension
- Roughly half of adults aged 65 years or older have prediabetes
Meanwhile, the American Diabetes Association estimates that 97% of those with prediabetes and 25% of diabetics go undiagnosed. This is not because prediabetes is difficult to diagnose; rather, diagnostic screenings do not occur as often as necessary.
Those who are obese represent a large market of motivated consumers who are actively searching for help on the Internet and encountering advice of variable quality and usefulness. Because there is not enough being done to screen for obesity-related preconditions, however, individuals with these conditions are too often not aware of nor connected with the behavioral support, nutritional guidance, coaching support, fitness tools, and other technologies they need to improve their health.
Community-Based Programs
Research findings demonstrate that programs incorporating behavioral counseling, dietary modification, and exercise can produce modest, yet meaningful sustained weight loss and result in significant improvements in health outcomes.
For example, the YMCA-based Diabetes Prevention Program has demonstrated that community-based lifestyle programs can help obese Americans lose weight and prevent progression to diabetes. This multiyear, national pilot program helped individuals with prediabetes in various locations around the country adopt healthier lifestyles. The program used face-to-face group meetings that included counseling, exercise sessions, and dietary advice. On average, participants achieved a modest mean 6% weight loss. This cut the rate of progression to diabetes over the course of several years by 58%, providing a great example of the effectiveness of community-based lifestyle programs.5
Coaching programs are also beginning to pop up in community pharmacies. Rite Aid, for example, is currently piloting a lifestyle-focused, face-to-face coaching program for those with known chronic disease. Under this Rite Aid Health Alliance program, in-store, integrated care team partners collaborate with local health care providers to help manage patients with poly-chronic conditions. Patients meet regularly with in-store care coaches and Rite Aid pharmacists to receive counseling on weight management, fitness, and medication adherence. Participants in this program have had considerable success with weight loss, diabetes, and hypertension control, as well as medication adherence.6
Convenient Care Programs
Convenient care clinicians are well situated to provide easily accessible, low-cost solutions for the diagnosis and treatment of obesity and its related conditions. RediClinic, which is a wholly owned subsidiary of Rite Aid, is a case in point.
Like most convenient care providers, RediClinic routinely screens patients for gaps in care and lifestyle issues such as smoking, drinking, and obesity. In addition, RediClinic offers a proprietary, medically supervised weight management program called Weigh Forward. David Katz, MD, MPH, FACPM, FACP, a renowned weight-loss expert and director and founder of Yale University’s Prevention Research Center, developed and directs this 10-week program that focuses on 4 key components of weight management: medical, behavioral, exercise, and diet and nutrition. Under the program, patients visit with a specially trained RediClinic clinician 15 to 30 minutes a week to discuss barriers and formulate solutions to make healthy lifestyle changes. The program has been successful in helping patients lose 1 to 2 pounds per week, while significantly improving their cardiometabolic health.
Health Plan Coverage for Programs
One significant barrier to making progress in the fight against obesity and its related chronic conditions is the lack of payer support. Historically, convenient care providers have introduced innovative services to the market by offering self-pay options, which eventually attract payer support. Hopefully, this is the path that Weigh Forward and other medically supervised weight management programs are now following.
Presently, most commercial payers reimburse for various services for morbidly obese patients. However, coverage for weight management services for those at earlier stages of obesity is spotty at best, usually consisting of discounts for various weight-loss programs. For this reason, it is always best for patients to contact their health plan to understand which services are covered.
However, there is reason to believe that change is coming. The Affordable Care Act requires many health plans to cover preventive services without a copay or deductible. Although this includes obesity counseling, there is no exact definition of what obesity counseling must include, and thus coverage varies from plan to plan.
Today, Medicare reimburses for weight management programs that meet certain criteria. About 30% of seniors are obese and would be eligible for reimbursable counseling services under existing Medicare policy. However, less than 1% of Medicare’s 50 million beneficiaries have used this benefit thus far. Experts blame the government’s failure to promote the program, as well as complex rules that limit when and where participants can go for weight-loss counseling.7
Conclusion
Obesity and sedentary lifestyles are the substrates that fuel the daunting epidemic of chronic disease. Much like the smoking epidemic, successfully battling obesity will require the participation of many stakeholders. Screening and treating individuals for very common preconditions is vital and can often occur outside the physician’s office.
Convenient care clinics are poised to play an integral role in identifying and addressing chronic disease risk factors. They are well suited to provide low-cost, efficient, and accessible screening, diagnostic, and treatment services for preconditions that, if left unaddressed, develop into the leading causes of death and disability in our country, as well as drivers of significant health care costs.
Peter Goldbach, MD, is the chief medical officer (CMO) of RediClinic and Health Dialog. As CMO of RediClinic, he is responsible for oversight of all clinical activities, including RediClinics’ credentialing, care protocols, continuous quality improvement initiatives, and treatment protocols. As CMO of Health Dialog, Peter is responsible for the clinical integrity of their coaching and shared decision-making programs, supporting the sales and marketing teams, and providing leadership in the development of new products. He is a board-certified specialist in pulmonary disease and had maintained a pulmonary and primary care practice.
References
- Accenture. Number of U.S. retail health clinics will surpass 2,800 by 2017, Accenture forecasts.newsroom.accenture.com/news/number-of-us-retail-health-clinics-will-surpass-2800-by-2017-accenture-forecasts.htm. Published November 12, 2015. Accessed May 10, 2016.
- Mehrotra A, Liu H, Adams JL, et al. Comparing costs and quality of care at retail clinics with that of other medical settings for 3 common illnesses.Ann Intern Med. 2009 Sep 1;151(5):321-328.
- Sturm R. The effects of obesity, smoking, and drinking on medical problems and costs.Health Aff (Millwood). 2002;21(2):245-253. doi: 10.1377/hlthaff.21.2.245.
- CDC. National diabetes statistics report, 2014: estimates of diabetes and its burden in the United States.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Published 2014. Accessed May 10, 2016.
- Ackermann RT, Finch EA, Brizendine E, Zhou H, Marrero DG. Translating the Diabetes Prevention Program into the community. The DEPLOY pilot study.Am J Prev Med. 2008 Oct;35(4):357-63. doi: 10.1016/j.amepre.2008.06.035.
- Health Dialog. Rite Aid health alliance results. info.healthdialog.com/white-paper-download-rite-aid-health-alliance-results. Published April 5, 2016. Accessed May 10, 2016.
- Galewitz P. Seniors’ obesity-counseling benefit goes largely unused.MedPage Today. medpagetoday.com/PublicHealthPolicy/Medicare/48753. Published November 20, 2014. Accessed May 10, 2016.