Diabetic Eye Exams: Why They Matter
Diabetes can result in vision problems, so it is important to closely monitor patients through comprehensive eye examinations.
Diabetes can result in vision problems, so it is important to closely monitor patients through comprehensive eye examinations.
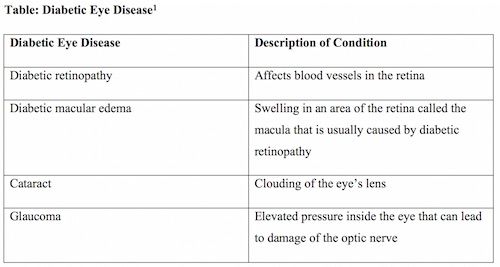
Unfortunately, diabetic eye disease may cause vision loss and blindness. Diabetic eye disease is a group of conditions that includes cataracts, diabetic macular edema, diabetic retinopathy, and glaucoma.
1
DIABETIC EYE DISEASE
Controlling blood glucose by exercising, maintaining a healthy diet, and taking medication can delay or prevent vision loss. Early detection, treatment, and close monitoring are essential to prevent vision problems in patients with diabetes (Table
). Diabetic retinopathy is the leading cause of vision loss, blindness, and vision impairment among patients with diabetes.
2
Chronic hyperglycemia, diabetes duration, diabetic kidney disease, dyslipidemia, and hypertension are among the factors that increase the risk of retinopathy.
3
Individuals may not develop symptoms in the early stages of diabetic retinopathy, but as the condition progresses, symptoms may include blurred vision, dark or empty areas in the vision, floaters, fluctuating vision, impaired color vision, and vision loss.
2
EYE EXAM RECOMMENDATIONS
The American Diabetes Association (ADA) recently issued updated recommendations on preventing, assessing, and treating diabetic retinopathy.
3
Evidence shows that optimizing blood pressure, glycemic control, and serum lipids can reduce the risk or slow the progression of diabetic retinopathy.
3
Additionally, the ADA recommends that adults with type 1 diabetes (T1D) should have an initial dilated and comprehensive eye examination by an ophthalmologist or an optometrist within 5 years of the onset of diabetes.
3
Patients with type 2 diabetes (T2D) should have this examination when they receive their diagnosis. If the exam shows no indication of retinopathy for at least 1 annual eye exam and blood glucose is well controlled, then eye exams every 1 to 2 years may be considered.
3
If there are signs of diabetic retinopathy, then
follow-up dilated retinal exams should be repeated at least annually.
3
Retinopathy progression and vision problems require more frequent eye exams. Women with preexisting T1D or T2D planning pregnancy or who are pregnant should be told about the risk of development and progression of diabetic retinopathy. Eye exams should occur before pregnancy or in the first trimester in patients with T1D, and individuals should be monitored every trimester and for 1 year postpartum based on the degree of retinopathy.
3
During a comprehensive eye exam, drops are used to dilate the eyes, and the following are assessed: abnormal blood vessels; swelling, blood, or fatty deposits in the retina; growth of new blood vessels and scar tissue; bleeding; retinal detachment; optic nerve abnormalities; vision; eye pressure for glaucoma; and signs of cataracts.
2
Retinopathy treatment may consist of panretinal laser photocoagulation therapy and intravitreous injections of the antivascular endothelial growth factor ranibizumab (Lucentis).
3
PHYSICIAN ASSISTANT INVOLVEMENT
Physician assistants can play a key role in treating patients with diabetes through an interdisciplinary approach that includes medication therapy management. Those who manage glycemic control through medication compliance can reduce their risk of diabetic retinopathy. Evidence has shown that pharmacist-managed diabetes clinics can offer positive outcomes related to diabetes quality measures.
4
Pharmacists can educate patients about comprehensive eye exams as part of their diabetes management and refer individuals to an ophthalmologist or an optometrist. Follow-up calls and pharmacist consults in the community setting may increase patient compliance with eye exams. As part of some pharmacy programs, students are trained in physical assessment, which includes basic eye exam principles and specialist referral education. Physical assessment courses are also offered as continuing education certificate programs that include identifying signs and symptoms of diabetic retinopathy.
Jennifer Gershman, PharmD, CPh, is a drug information pharmacist and Pharmacy Times®contributor who resides in south Florida.
References
- National Eye Institute. Facts about diabetic eye disease.nei.nih.gov/health/diabetic/retinopathy. Updated September 2015. Accessed August 17, 2018.
- Mayo Clinic. Diabetic retinopathy.mayoclinic.org/diseases-conditions/diabetic-retinopathy/symptoms-causes/syc-20371611. Published May 30, 2018. Accessed August 17, 2018.
- Introduction: standards of medical care in diabetes-2018.Diabetes Care.2018;41(suppl 1):S1-S2. doi: 10.2337/dc18-Sint01.
- Aneese NJ, Halalau A, Muench S, Shelden D, Fett J, Lauster C. Impact of a pharmacist-managed diabetes clinic on quality measures.Am J Manag Care.2018;24(4 Spec No.):SP116-SP119.
Knock Out Aches and Pains From Cold
October 30th 2019The symptoms associated with colds, most commonly congestion, coughing, sneezing, and sore throats, are the body's response when a virus exerts its effects on the immune system. Cold symptoms peak at about 1 to 2 days and last 7 to 10 days but can last up to 3 weeks.
COPD: Should a Clinician Treat or Refer?
October 27th 2019The Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines the condition as follows: “COPD is a common, preventable, and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases.â€
Diabetic Ketoacidosis Is Preventable With Proper Treatment
October 24th 2019Cancer, diabetes, and heart disease account for a large portion of the $3.3 trillion annual US health care expenditures. In fact, 90% of these expenditures are due to chronic conditions. About 23 million people in the United States have diabetes, 7 million have undiagnosed diabetes, and 83 million have prediabetes.
What Are the Latest Influenza Vaccine Recommendations?
October 21st 2019Clinicians should recommend routine yearly influenza vaccinations for everyone 6 months or older who has no contraindications for the 2019-2020 influenza season starting at the end of October, according to the Advisory Committee on Immunization Practices.
What Is the Best Way to Treat Pharyngitis?
October 18th 2019There are many different causes of throat discomfort, but patients commonly associate a sore throat with an infection and may think that they need antibiotics. This unfortunately leads to unnecessary antibiotic prescribing when clinicians do not apply evidence-based practice.