Chronic Bronchitis
Chronic bronchitis is a common disease process that can lead to debilitating lung function and an increase in mortality.
Chronic bronchitis is a common disease process that can lead to debilitating lung function and an increase in mortality. According to the CDC, there are approximately 8.7 million adults diagnosed with chronic bronchitis and nearly 285,000 related visits to the emergency department each year.1The condition affects men more than women, and the majority of patients are between 44 and 65 years of age.2Accurate diagnosis and appropriate management of chronic bronchitis allow for improved patient outcomes.
Differentiating Acute from Chronic Bronchitis
Signs and symptoms of acute bronchitis are persistent cough that lasts 10 to 20 days, wheezing, low-grade fever, and chest tightness or pain. Although acute bronchitis lasts from a few days to 10 days, coughing can last for several weeks after the infection has subsided. The infection typically develops after a patient has recently had a cold or the flu virus.3Antibiotics are not commonly prescribed for acute bronchitis because the most common cause are viruses.
Chronic bronchitis is defined as a persistent cough and sputum production for at least 3 months per year for 2 consecutive years.2Common signs and symptoms of chronic bronchitis are coughing, wheezing, and chest discomfort. The cough can also produce a large amount of mucus (see Figure3), which is commonly referred to as a smoker’s cough.
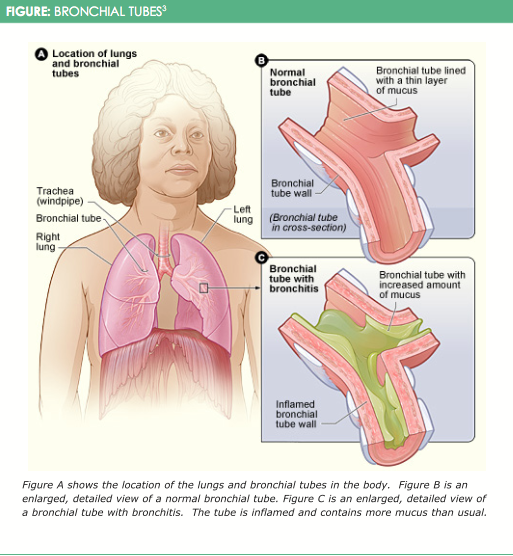
Although smoking is the number one cause, breathing in air pollution, dust, or fumes can also cause chronic bronchitis. Chronic bronchitis is caused by an overproduction and hypersecretion of mucus by goblet cells, also referred to as mucous metaplasia. Mucous hypersecretion largely develops as a result of cigarette smoke exposure, acute or chronic viral infection, or bacterial infection. Mucous metaplasia is further worsened by difficulty in clearing secretions due to poor ciliary function, distal airway occlusion, and ine ective cough attributable to respiratory muscle weakness and reduced peak expiratory flow.2Patients’ who have a history of chronic bronchitis typically go through periods when their symptoms are worse, which can be caused by a viral or bacterial infection.3Recent study results indicate that antibiotics are warranted in some cases of acute exacerbations of chronic bronchitis.
Diagnosis
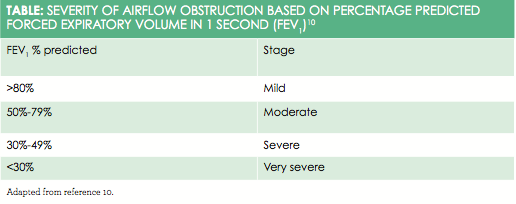
Proper diagnosis and evaluation of chronic bronchitis include pulmonary functions tests (PFTs; spirometry, diffusing capacity, and arterial blood gases). The standard PFTs should include pre- and postbronchodilator testing to conclude whether there is a response to the bronchodilator.4A measured forced expiratory volume in 1 second (FEV1) of less than 70 percent of the total forced vital capacity (FVC) (the FEV1/FVC ratio) defines obstructive airway disease. A FEV1/FCV ratio of less than 50 percent indicates endstage obstructive airway disease. The different levels of severity of airflow obstruction based on FEV1 can be seen in Table10.
Airflow obstruction along with the presence of chronic sputum production confirms the diagnosis of chronic bronchitis.5Chest x-rays may reveal increased lung markings in the lower lobes and peribronchial thickening in patients with chronic bronchitis.4To check for deficiency, a serum alpha1—antitripsin level should be performed if the patient is younger than 45 years, is a nonsmoker, or has a family history of young-onset of chronic bronchitis. During acute exacerbation of chronic bronchitis, a sputum culture and sensitivity should be performed to confirm the type of bacteria and susceptibility to an antibiotic treatment plan.4The most common pathogens seen in acute exacerbations of chronic bronchitis areH. influenzae,S. pneumoniae, andM. catarrhalis.6Yearly spirometry, complete blood count with differential, chemistry profile, and chest x-ray should be done to monitor the patient’s decline in pulmonary function and to screen for other lung diseases that may be related to smoking. Pulse oximetry can be done sporadically to assess for hypoxemia. Arterial blood gases should be performed if a pulse oximetry reading is less than 90 percent.4
Management
Risk Factors
Smoking is the number one modifiable risk factor. Encouraging patients to stop smoking and providing them with tools for smoking cessation has shown enormous benefits in improving chronic bronchitis. Second, removing air pollutants such as secondhand smoke, dust, and toxic gases in the environment or workplace can also improve the condition.7Another potential risk factor for chronic bronchitis is gastroesophageal reflux. Repeated reflux can lead to aspiration which can potentially cause acid-induced injury and infection that trigger bronchoconstriction and irritation of esophageal mucosa.8
Medications
Short-acting beta-adrenergic receptor agonists (SABAs) are the first line of chronic bronchitis therapy because they promote mucus clearance and prevent bronchospasm. Every time a patient experiences a bronchospasm it causes permanent alteration of the bronchioles, so preventing this is key. SABAs are used as “rescue” medications for shortness of breath. Some examples of SABA medications include albuterol (ProAir HFA, Proventil, Ventolin HFA) and levalbuterol (Xopenex). Long-acting beta agonists (LABAs) are not first-line treatments for chronic bronchitis, but they can be used as maintenance therapy. Overall, LABAs have mucociliary function. They also reduce hyperinflation and increase peak expiratory flow, both of which lead to a more effective cough, allowing patients to clear mucus more easily. Due to black box warnings on LABAs, they are also to be taken with an inhaled steroid. Examples of LABAs include salmeterol (Serevent) and formoterol (Foradil). Evidence has been found that salmeterol can specifically stimulate ciliary beat frequency. Likewise, one study’s results showed that formoterol, compared with placebo, can significantly improve mucus clearance in chronic bronchitis patients.4,5
Inhaled anticholinergic bronchodilators, such as ipratropium bromide (Atrovent) and tiotropium (Spiriva), used to be recommended for treatment of chronic bronchitis. Although the mechanism of action is to stimulate mucus clearance by means of bronchodilation, results from newer research studies indicate that inhaled anticholinergics desiccate airway secretions so much that expectorating secretions becomes difficult. For this reason, the literature does not support the use of anticholinergics for chronic bronchitis.5
Inhaled corticosteroids such as beclomethasone (Beclodisk), budesonide (Pulmicort), uticasone (Flovent), and triamcinolone (Azmacort) can be effective in management of chronic bronchitis due to their anti-inflammatory properties. Inhaled corticosteroids combined with LABAs are more effective to prevent bronchoconstriction and inflammation. Always educate your patient regarding good inhaler technique and mouth rinsing postinhalation to prevent oral candidiasis.4Systemic steroids may also be used in rare cases when a patient who has chronic bronchitis presents with an acute exacerbation, as discussed in the next section.
Saline, steam, or other agents have not been proven to aid in mucociliary clearance or expectoration. Oral expectorants such as guaifenesin (Robitussin, Mucinex) are usually ineffective as well. A systematic review of 34 studies showed only a small decrease in the number of acute exacerbations in chronic bronchitis when using a mucolytic regularly.8
Acute Exacerbations of Chronic Bronchitis
Acute exacerbations of chronic bronchitis include the following 3 symptoms: increase in baseline dyspnea, increase in sputum volume, or appearance of purulent expectorations. The severity of these acute exacerbation symptoms can be graded using the Anthonisen severity criteria: type I includes presence of all 3 symptoms, type II includes presence of 2 of the 3 symptoms, and type III includes presence of 1 of the 3 symptoms. Antibiotic therapy is necessary in type I and type II acute exacerbation. Antibiotic therapy is not needed in a type III acute exacerbation. Due to increasing antibiotic resistance and overprescription, a shorter course of antibiotic therapy is desirable if prescribed for type I or II. Several studies have compared 5-day, 7-day, and 10-day antibiotic therapy for chronic bronchitis. They found that the length of treatment demonstrated equivalence in clinical efficiency and cure rates.9According to Cleveland Clinic, due to emerging antibiotic resistance, second-generation macrolides and second- and third-generation cephalosporins are preferred treatments for acute exacerbations of chronic bronchitis over the traditional first-line antibiotics (doxycycline and trimethoprim-sulfamethoxazole).6
Oxygen Therapy
This is helpful in relieving the hypoxia associated with chronic bronchitis. Requirements for home oxygen include a PaO2 of 55 mm Hg or less or oxygen saturation below 85% and a PaO2 of 55 to 59 mm Hg if any of the following is present: erythrocytosis, cor pulmonale, edema, or CHF. The goal of oxygen therapy is a PaO2 of 60 mm Hg or oxygen saturation of 90%. This can typically be met with 1 to 2 L of oxygen per minute for 15 hours per day.4
Lifestyle Modifications
Walking or bicycling can significantly promote respiratory muscle conditioning in patients with chronic bronchitis. Washing hands frequently and following a healthy diet are vital to lowering the risk of bacterial or viral infections.
Patient Education
Patients should avoid extreme temperature and humidity changes, as well as limit visits to areas of air pollution. Smoking cessation is a must. Smoking should not be present in the home, car, or any other confined area. Traveling at high altitudes or in airplanes can be a risk for patients with hypoxemia. Avoid large crowds during flu season. Patients should receive the influenza and pneumonia vaccine as preventative measures. Walking and bicycling are the best exercises to strengthen respiratory muscles and aid in expectorating mucus. During acute attacks, patients should be educated on how to use pursed-lip breathing to help decrease their respiratory rate, reduce bronchospasm, and relieve dyspnea. Coughing and deep-breathing techniques as well as chest physiotherapy are also useful. Support groups are available for patients if they are struggling with the diagnosis. Unstable or uncontrolled patients should be seen monthly. Stable patients with chronic bronchitis can be seen yearly.4
Conclusion
Chronic bronchitis is a despairing disease process, and it is 1 of the 5 leading causes of death worldwide.9Differentiating between acute and chronic bronchitis is the first step to proper diagnosis and management. Smoking is the leading cause of chronic bronchitis. Implementing smoking cessation education and encouraging patients to stop smoking is essential. Providing a supportive relationship with the patient allows a practitioner to verbalize the necessity for smoking cessation during each visit. Proper diagnosis and management of chronic bronchitis in patients is crucial for ultimately decreasing their decline in lung function, acute exacerbations, and mortality.
Tiffany Budzinskiis aboard-certified family nurse practitioner specializing in retail health. She currentlyworks for CVS MinuteClinic. She earned her bachelor of sciencein nursing degree at University of Illinoisin Chicago and her masters of science in nursing at Saint Xavier University in Evergreen Park, Illinois.
References
- Chronic obstructive pulmonary disease includes: chronic bronchitis and emphysema. CDC website. cdc.gov/nchs/fastats/copd.htm. October 7, 2016. Accessed February 21, 2017.
- Kim V, Criner G. Chronic Bronchitis and Chronic Obstructive Pulmonary Disease.Am J Respir Crit Care Med.2013;187(3):228-237. doi: 10.1164/rccm.201210-1843CI.
- National, Heart, Lung and Blood Institute. What is Bronchitis? Department of Health and Human Services; National Institutes of Health website. www.nhlbi.nih.gov/health/health-topics/topics/brnchi. Updated August 4, 2011. Accessed February 21, 2017.
- Dunphy L, Winland-Brown J, Porter B, Thomas D.Primary Care: The Art & Science of Advanced Practice Nursing.3rd ed. Philadelphia, PA:FA.Davis; 2011.
- Heath J, Mongia R. Chronic bronchitis: primary care management.Am Fam Physician.1998;57(10):2365-2372.
- Budey M, Wiedemann HP. 2010.Acute Bacterial Exacerbation of Chronic Bronchitis.Cleveland Clinic Continuing Education website. clevelandclinicmeded.com/medicalpubs/diseasemanagement/pulmonary/acute-bacterial-exacerbation-chronic-bronchitis/. Published August 1, 2010. Accessed February 21, 2017.
- Bronchitis. Mayo Clinic website. mayoclinic.org/diseases-conditions/bronchitis/basics/definition/con-20014956. Published April 1, 2014. Accessed February 21, 2017.
- Poole P, Chong J, Cates CJ. Mucolytic agents versus placebo for chronic bronchitis or chronic obstructive pulmonary disease (review).Cochrane Database Syst Rev.2015:7:CD001287. doi: 10.1002/14651858.CD001287.pub5.
- Bashlian R, Sun C, Dorsen, C. Short- vs long-course antibiotics for acute exacerbations of chronic bronchitis.J Nurse Pract.2012;8(7):534-539.
- Ranu H, Wilde M, Madden B. Pulmonary function tests.Ulster Med J.2011; 80(2):84-90.