The Low-Down on Low Back Pain
Low back pain (LBP) is the fifth most common reason for all primary care visits, and 6 million Americans see primary care providers complaining of LBP annually.
Low back pain (LBP) is the fifth most common reason for all primary care visits, and 6 million Americans see primary care providers complaining of LBP annually. It is also one of the most expensive conditions to manage if it becomes chronic.
Retail health care providers are likely to see patients who have LBP complaints. The typical patient reporting a first episode of LBP is between the ages of 20 and 40, and the incidence increases after age 40. For most patients—a full 85%–symptoms will resolve within 2 weeks, and they are diagnosed with acute LBP. For the remaining 15%, back pain can become a chronic condition that is extremely difficult to treat.
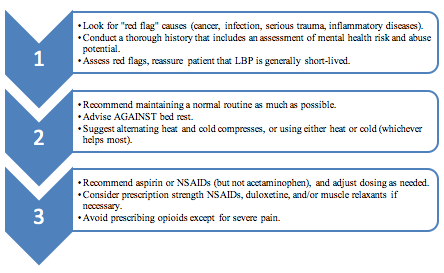
Numerous evidence-based guidelines are available that address LBP. The two that clinicians employ most often are the American College of Physicians guidelines, updated in April 2017, and the NICE guidelines. Both guidelines make similar recommendations, as described in Figure 1.
Figure 1. Streamlined Approach to Low Back Pain
Many health care providers have little confidence that they can treat LBP efficiently and effectively, especially if it becomes chronic. Guidelines suggest reasonable and rational approaches, but health care providers may be unfamiliar with the guidelines or have difficulty interpreting them. In particular, the guidelines suggest a number of distinct interventions, but health care providers find that they are not very clear about using treatments in combination. With most patients, clinicians need to use several interventions that meet their unique needs. Understanding that patients who have LBP often also suffer from depression, sleep disturbances, and anxiety can help too.
Treating LBP in retail health care clinics is prudent because it is less expensive than specialist care. Guideline adherence can reduce costs further. One area that's been identified as critical to improving care in primary care settings is counseling patients about effective self-management and exercise, over-the-counter interventions like heat pads, and massage. Further, addressing the patient's depression or anxiety is very important.
Recent changes to guidelines and recommendations that clinicians often ignore include the following:
- Bedrest is not an appropriate intervention for LBP. Patient should try to maintain their activity levels, avoiding only activities that cause or aggravate pain. "Keep moving" is excellent advice.
- Patients who present with a first episode of LBP usually do not need imaging.
- Acetaminophen is not an effective intervention for LBP. Aspirin or the nonsteroidal anti-inflammatory drugs are better choices.
- Many patients who experience LBP are also taking other drugs or have comorbidities. It's critical to screen for medication-related problems in advance of recommending OTC analgesics or prescribing new medications.
- Opioids are a last resort for pain management and LBP. This is a critical fact since rates of opioid prescribing for LBP have rocketed in the last 2 decades.
- Patients with concurrent diagnoses of depression are twice as likely prescribed opiates for LBP, usually receive more than twice the typical dose to relieve their pain, and are at highest risk for opioid misuse and overdose.
LPB consumes more than $86 billion of the annual health care budget in the United States. It also increases the risk of unnecessary exposure to unproven opioid prescriptions and can perpetuate prolonged exposure and addictions in these individuals. Knowing that LPB will resolve within 2 weeks in most cases can help clinicians and patients find simple, effective interventions.
Reference
Abdel Shaheed C, Maher CG, Williams KA, et al. Efficacy, tolerability, and dose-dependent effects of opioid analgesics for low back pain: a systematic review and meta-analysis.JAMA Intern Med. Available at: http://archinte.jamanetwork.com/article.aspx?articleid=2522397. Accessed January 22, 2018.
NICE. Low Back Pain and Sciatica in Over 16s: Assessment and Management. National Institute for Health and Care Excellence: Clinical Guidelines. 2016. London: National Institute for Health and Care Excellence (UK), 2016.
Qaseem A, Wilt TJ, McLean RM, et al. Clinical Guidelines Committee of the American College of Physicians. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians.Ann Intern Med.2017;166(7):514-530.
