Probiotics Play Key Role in the Gastrointestinal Tract
The live organisms help maintain immunologic equilibrium through direct interaction with immune cells.
Probiotics are live organisms that have a symbiotic relationship with the body, most often in the gastrointestinal (GI) tract.
The most common probiotics included in various formulations are bidifobacteria, lactobacilli, and the yeast Saccharomyces boulardii. Probiotics are available in a wide range of products, formulations and strains.
Evidence indicates that certain probiotics are possibly effective for GI conditions, such as antibiotic-associated diarrhea, chronic pouchitis associated with ulcerative colitis, constipation, diarrhea in adults and children, Helicobacter pylori in conjunction with standard therapies, irritable bowel syndrome (IBS), and reducing the risk of C. difficile infection.
The natural medicines database generally defines a “possibly effective” rating as “some clinical evidence supporting its use for a specific indication.”
However, the evidence is limited by quality, quantity, or contradictory findings.
Products rated “possibly effective” might be beneficial but do not have enough high-quality evidence to recommend for most individuals.1
In 2020, the American Gastroenterological Association (AGA) published clinical practice guidelines on the role of probiotics for gastrointestinal diseases.2 The AGA concluded that certain probiotics may be beneficial for preventing C. difficile in patients taking antibiotics, but the quality of evidence was low and thus required further study. The AGA concluded similar findings for effectiveness of probiotics in patients with IBS and inflammatory bowel disease (IBD). An 8-strain combination probiotic including various lactobacillus and bifidobacteria species was helpful in patients with pouchitis related to IBD. Evidence also supported the use of certain bifidobacterial- and lactobacilli-containing probiotics in preterm infants to prevent necrotizing enterocolitis.
Probiotics are safe and well tolerated when taken appropriately in generally healthy people. There are some reports of mild GI effects, such as bloating, diarrhea, and flatulence.3,4
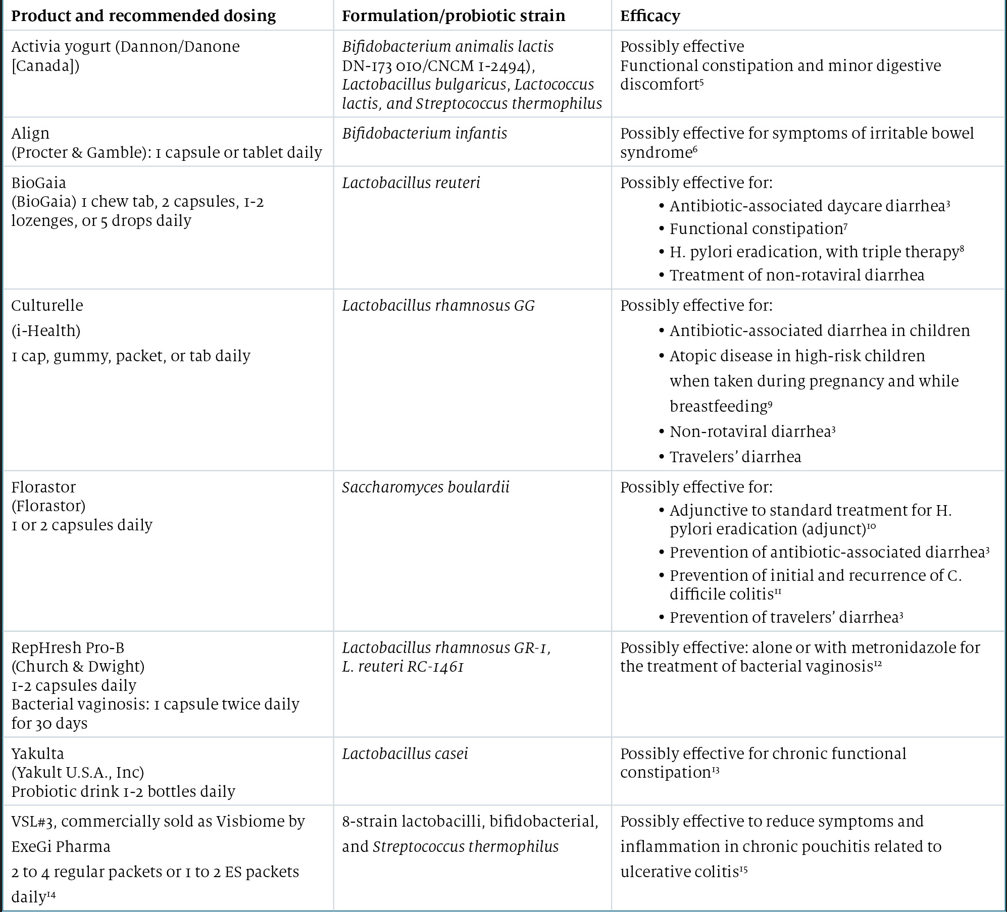
The Table3 5-15 summarizes the most commonly used probiotics.
Table. Common Probiotic Products, Formulation/Strains, and Overview of Clinical Efficacy3, 5-15
Conclusion
Probiotics play a key role in the maintenance of immunologic equilibrium in the gastrointestinal tract through the direct interaction with immune cells. There is high-quality evidence that probiotics are effective for acute infectious diarrhea, antibiotic-associated diarrhea, Clostridium difficile–associated diarrhea, functional constipation, H pylori eradication, and IBS. Probiotics may improve human health, nutrition, and regulation of common GI abnormalities.
References
1. Editorial principles and process. Natural Medicines. Accessed April 3, 2022. https://naturalmedicines.therapeuticresearch.com/about-us/editorial-principles-and-process.aspx
2. Su GL, Ko CW, Bercik P, et al. AGA clinical practice guidelines on the role of probiotics in the management of gastrointestinal disorders. Gastroenterology. 2020;159(2):697-705. doi:10.1053/j.gastro.2020.05.059
3. Probiotics. What works and what doesn’t. Natural Medicines. March 20, 2020. Accessed August 1, 2022. https://naturalmedicines.therapeuticresearch.com/news/news-items/2020/march/probiotics-what-works-and-what-doesn%E2%80%99t.aspx
4. Comparison of common probiotic products. Pharmacist’s Letter. Accessed April 3, 2022. https://pharmacist.therapeuticresearch.com/Content/Segments/PRL/2015/Jul/Comparison-of-Common-Probiotic-Products-8626
5. Guyonnet D, Schlumberger A, Mhamdi L, Jakob S, Chassany O. Fermented milk containing bifidobacterium lactis DN-173 010 improves gastrointestinal well-being and digestive symptoms in women reporting minor digestive symptoms: a randomized, double-blind, parallel, controlled study. Br J Nutr. 2009;102;1654-1662. doi:10.1017/S0007114509990882
6. Whorwell PJ, Altringer L, Morel J, et al. Efficacy of an encapsulated probiotic Bifidobacterium infantis 35624 in women with irritable bowel syndrome. Am J Gastroenterol. 2006;101:1581-1590. doi:10.1111/j.1572-0241.2006.00734.x
7. Riezzo G, Orlando A, D'Attoma B, Linsalata A, Martulli M, Russo F. Randomized double-blind placebo-controlled trial on Lactobacillus reuteri DSM 17938: improvement in symptoms and bowel habit in functional constipation. Benef Microbes. 2018;9(1):51-60.doi:10.3920/BM2017.0049
8. Poonyam P, Chotivitayatarakorn P, Vilaichone RK. High effective of 14-day high-dose PPI- bismuth-containing quadruple therapy with probiotics supplement for helicobacter pylori eradication: a double blinded-randomized placebo-controlled study. Asian Pac J Cancer Prev. 2019;20(9):2859-2864. doi:10.31557/APJCP.2019.20.9.2859
9. Blaabjerg S, Artzi DM, Aabenhus R. Probiotics for the prevention of antibiotic-associated diarrhea in outpatients: a systematic review and meta-analysis. Antibiotics. 2017;6(4):21. doi:10.3390/antibiotics6040021
10. Zhou BG, Chen LX, Li B, Wan LY, YW A. Saccharomyces boulardii as an adjuvant therapy for Helicobacter pylori eradication: a systematic review and meta-analysis with trial sequential analysis. Helicobacter. 2019;24(5):e12651. doi:10.1111/hel.12651
11. Johnston BC, Lytvyn L, Lo CK, et al. Microbial preparations (probiotics) for the prevention of clostridium difficile infection in adults and children: an individual patient data meta-analysis of 6,851 participants. Infect Control Hosp Epidemiol. 2018;39(7):771-781. doi:10.1017/ice.2018.84
12. Wang Z, He Y, Zheng Y. Probiotics for the treatment of bacterial vaginosis: a meta-analysis. Int J Environ Res Public Health. 2019;16(20):3859. doi:10.3390/ijerph16203859
13. Dimidi E, Christodoulides S, Fragkos KC, Scott SM, Whelan K. The effect of probiotics on functional constipation in adults: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr. 2014;100(4):1075-1084. doi:10.3945/ajcn.114.089151
14. Visbiome. Product inserts. Accessed August 1, 2022. https://www.visbiome.com/pages/product-inserts
15. Gionchetti P, Rizzello F, Venturi A, et al. Oral bacteriotherapy as maintenance treatment in patients with chronic pouchitis: a double-blind, placebo-controlled trial. Gastroenterology. 2000;119(2):305-309. doi:10.1053/gast.2000.9370
