Nurse Practitioners' Hep C Treatment Equally Effective as Specialist Care
Given the limited access to hepatitis C virus (HCV) specialists, nurse practitioners and physician assistants should begin to manage HCV in the community setting.
Given the limited access to hepatitis C virus (HCV) specialists, nurse practitioners and physician assistants should begin to manage HCV in the community setting.
A recent, multi-center, open label, phase 4 study involving 600 patients demonstrated that nurse practitioners and physician assistants are capable health care providers for patients infected with HCV.
The researchers sought to learn more about the efficacy and safety of HCV care by nonspecialists. They enrolled patients from 2 community health centers in Washington, DC, and separated them into 3 treatment groups:
- A nurse practitioner group
- A primary care physician group
- A specialist in infectious disease or hepatology group
Of the 600 participants in the cohort, 578 (96.3%) were African-American. The average age was around 58 years, and the majority of the participants were men and treatment-naïve. Around 140 of the participants had HCV and HIV co-infection.
Around 70 of the 600 study participants discontinued therapy early. A little more than 50 were lost to follow up, 7 discontinued following providers’ orders, 5 discontinued on their own accord, 3 participants died, and 3 discontinued due to provider-noncompliance.
The researchers also collected information about the participants’ adherence to the visits at 4, 8, 12, and 24 weeks, and those who saw nurse practitioners had the best visit adherence percentages overall.
Cumulative visit adherence was 81.5% for the patients who saw nurse practitioners versus 76.8% for those treated by primary care physicians and 63.8% for those treated by specialists.
All of the providers involved in the ASCEND study completed 3-hour training on guidelines from the American Association for the Study of Liver Diseases and Infectious Diseases Society of America.
Patients were treated with ledipasvir and sofosbuvir, and the primary outcome was unquantifiable HCV RNA viral load 12 weeks after the patients completed the therapy.
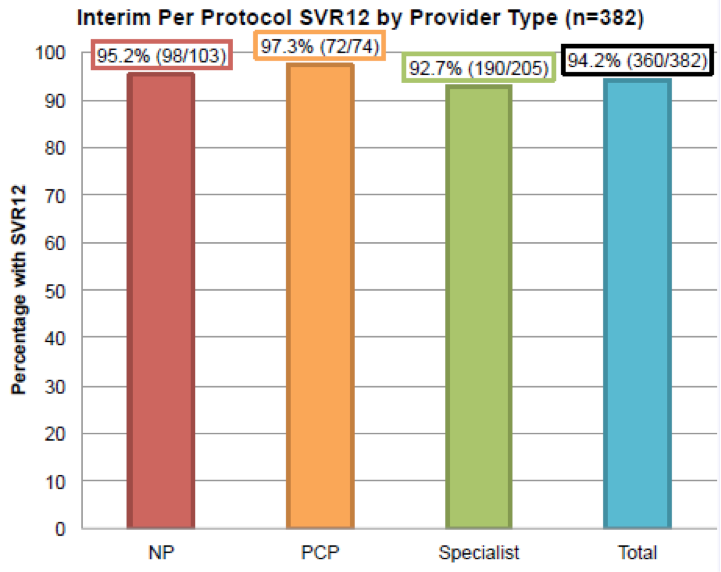
Of the 332 patients who met label criteria for an 8-week duration of treatment, only 29 were treated for 8 full weeks. Around 530 patients were treated for 12 weeks, and 32 were treated for 24 weeks. Of the 382 patients with available SVR12 results, around 94% achieved SVR12.
The researchers found that the nurse practitioners achieved statistically the same rate of sustained virologic response as the specialists.
“I was not surprised by these findings, given the complex and specialized medical care that most nurse practitioners and physician assistants provide in the modern era,” lead study author Sarah M. Kattakuzhy, MD, of the Institute of Human Virology at the University of Maryland, toldContemporary Clinic. “Given the advent of simple therapeutic options, along with consensus guidelines, I do expect more nurse practitioners and physician assistants will care for HCV in community-based settings.”
However, Dr. Kattakuzhy pointed out that insurance restrictions around prescribers could limit their involvement in some states.
“As the ASCEND study indicates, this restriction is not evidence-based and creates an additional hurdle in access to care,” she said.
Based on their findings, the researchers asserted that community-based, nonspecialist care for HCV therapy could close gaps in care.
“The ASCEND investigation demonstrates that HCV treatment administered independently by primary care physicians and nurse practitioners is safe and equally effective as care observed with experienced specialists, inclusive of challenging subpopulations of the epidemic, and within the largest black cohort described to date,” the researchers stated.
