Drug Devices: Education at Every Level
Some medications need a little help to be effective.
Some medications need a little help to be effective.
Medications that use a machine, device, or vehicle for administration are considered drug delivery devices.1Proper use of these devices is essential for maximal therapeutic benefit.2
Retail clinics are ubiquitous, with more than 1800 clinics providing more than 10 million visits annually.3Originally envisioned for acute care, these clinics are now frequently providing prescription refills.4
Additionally, many retail clinics offer chronic disease care, so retail clinicians see patients with asthma, diabetes, and lipid disorders.5
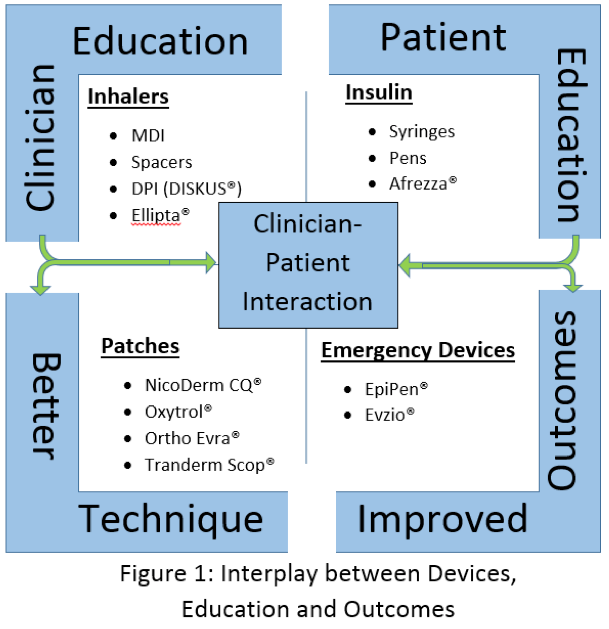
This changing focus increases the need for education for patients, as well as providers (Figure 1).
Devices for Asthma Management
Asthma is a $50 million problem annually, affecting 25 million Americans.6,7Inhalers remain the cornerstone treatment for asthma, although nebulizers are also used.
Device selection is critical and should be tailored to patients’ abilities.8In fact, poor inhaler technique is the main cause of treatment failure.9Alarmingly, 40% to 67% of health care providers are ill-equipped to teach their patients proper inhaler technique.10
Metered-Dose Inhalers
Metered-dose inhalers are used most often in asthma management.11The devices are sleek, but their use is not intuitive.
For example, patients must shake their metered-dose inhalers before use to disperse the drug evenly in its propellant. Then, they must remove the cap, exhale, and gently bite the mouthpiece while using their lips to make a tight seal.
Patients should tilt their head back slightly and begin to inhale slowly through their mouth, and then press the canister while continuing to inhale a full breath. Next, they should remove the inhaler from their mouth and hold their breath for 10 seconds to ensure proper drug settling.
Retail clinicians must remind patients to clean their inhaler’s plastic parts (not the canister) at least once a month with mild soap and water, and then air dry it. After reassembly, advise a test dose to be certain it is assembled correctly.12
Spacers are recommended for metered-dose inhalers that contain inhaled corticosteroids for 2 reasons: they increase the amount of medication reaching the lungs, and they decrease medication deposition in the back of the throat.
To use a spacer, patients remove the inhaler and spacer caps and then insert the inhaler mouthpiece into the spacer. Retail clinicians should instruct patients to place the spacer’s mouthpiece like they would a metered-dose inhaler and press on the canister.
Patients must inhale slowly and steadily once, fully filling the lungs. Remind patients to clean the spacer periodically to avoid static charge, which can attract drug particles. After disassembly, patients should rinse the spacer and allow it to air dry.13
Dry-Powder Inhalers
Dry-powder inhalers are also common in asthma management, with the Diskus inhaler being prescribed most often.
Retail clinicians should show patients how to slide the protective cover back to expose the mouthpiece using the thumb grip. Patients should hold the Diskus in their dominant hand with the mouthpiece facing them.
Using their dominant thumb, patients will slide the lever back until it clicks. Patients should hold the Diskus horizontal and breathe in quickly and deeply.
Here, too, instruct patients to hold their breath for 10 seconds and then exhale. Cleaning the device with a dry tissue or cloth is simple.14
The FDA approved a new one-step dry-powder inhaler, the Ellipta device, in 2013.
To use Ellipta, patients slide the cover open to expose the mouthpiece. They should exhale completely and then place the mouthpiece in their mouth, tilt the chin up slightly, and inhale slowly and deeply.
Note that this device has air vents that allow patients to breathe more normally. Like the other devices, patients need to hold their breath for 10 seconds and then exhale through the nose. Cleaning is the same as other dry-powder inhalers.15
Up to 94% of asthma patients misuse their inhalers. A study of 4078 asthma patients showed that patients who always used inhalers correctly had a lower asthma instability scores. Studies have shown that 25% of asthma patients never receive verbal instruction on how to use their inhaler and one-half receive one session of 10 minutes or less.10
Based on these statistics, we can do better!
Devices for Diabetes Management
Diabetes affects 30 million Americans and costs $245 billion annually. In fact, a diabetic patient costs the health care system 2.3 times more than a person without a diabetes diagnosis.
With an estimated 6 million Americans using insulin, teaching patients how to use their insulin delivery devices is critical.16
Insulin was first introduced in 1922 using syringes and vials, which were the only ways to administer insulin for 60 years. In the 1980s, insulin pens changed diabetics’ treatment.17
Although insulin pens are becoming more popular, syringes are still used despite their complexity. Retail clinicians are usually trained to teach patients with diabetes how to inject insulin, but even with proper instruction, patients struggle with syringes’ multiple steps and pieces of equipment.
Patients often forget to inject air into the vial before pulling up the dose. Air bubbles are inevitable and frustrating.
Patients also need guidance about used needle disposal, though newer devices eliminate these complications.18
Insulin Pens
Patients much prefer small, easy-to-use insulin pen needles. Instruct patients to remove the cover and gently roll the pen between the hands for 15 seconds to mix its contents thoroughly.
Next, patients should remove the foil cover of a pen needle and screw the needle to the top of the pen. Remove the outermost cover, but do not throw it away.
After the inner cap is removed and discarded, insulin pens must be primed. To do so, patients will hold the needle vertically with the needle pointing up. Then, they must dial the knob to the number 2 and press the knob up, watching the needle to ensure insulin comes out.
Now, the needle is ready for use. Next, patients dial the knob until the desired dose appears in the dose window.
Patients should clean a small area on the abdomen (about 3 inches to the right or left of the naval) with an alcohol pad. Once dry, they should pinch the injection area and insert the needle.
To release the dose, they must press down on the knob and hold the needle in place for 10 seconds. Then, they remove and re-cap the needle and twist the used needle off.
Much like syringes, proper needle disposal is needed.19If patients do not have a sharps container, they can use empty, thick plastic laundry detergent bottles.20
Inhalable Insulin
Approved in 2014, Afrezza is the first inhalable insulin. The small, whistle-like device is user-friendly (Figure 2).

Patients should find the appropriate dose cartridge and warm it at room temperature for 10 minutes before use. Patients open the device by pulling up on the mouthpiece. Then, they insert the dose cartridge.
Once loaded, the inhaler needs to be held level. To close the inhaler, they reverse the process and pull down on the mouthpiece and listen for the snap.
To administer the dose, patients remove the mouthpiece cover, exhale completely, and then place the mouthpiece between the teeth, wrapping lips firmly around it with the head straight.
They must tilt the inhaler down towards the chin slightly and then inhale deeply, remove the inhaler, and hold their breath as long as comfortable. To finish, patients replace the mouth cover and discard the used cartridge.
Retail clinicians should emphasize Afrezza storage. Patients must refrigerate unopened foil packages and use packages that come to room temperature within 10 days. Inhalers must be replaced every 15 days.21
Transdermal Patch
A transdermal patch is a drug loaded into a reservoir or matrix and applied to the skin for local or systemic absorption.
Transdermal patches are common in clinics and retail settings, often as OTC drugs. One billion patches are manufactured each year to treat more than 20 different conditions (Table).22
Patches
Indication
Type of Patch
Dose
Clinical Counseling Point
NicoDerm CQ
Smoking cessation
Reservoir
Step 1: 21 mg/24 hr
Step 2: 14 mg/24 hr
Step 3: 7 mg/24 hr
Smoke >10 cigarettes a day start with step 1
Smoke <10 cigarettes a day start with step 2
Apply new patch daily
Oxytrol
Over Active Plater
Matrix
3.9 mg/24 hours
Apply new patch every 3 to 4 days
Ortho Evra
Contraception
Matrix
150-35 mcg/24 hours
Apply one patch to the skin every week for 3 weeks. Then do not apply a patch for a week and begin again the following week.
Transderm Scop
(scopolamine)
Motion Sickness
Reservoir
1mg/24 hours
Apply one patch behind the ear 4 to 12 hours prior to anticipated need. Replace patch every 72 hours as needed.
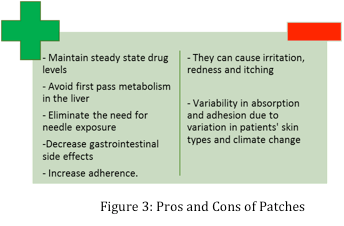
Patches offer many benefits, in addition to a few pitfalls (Figure 3).23
Patches come in 2 main types: reservoir and matrix.
Reservoir patches deliver drug to the skin using a controlled-release membrane.22Cutting these patches disrupts the release mechanism, making them ineffective and potentially dangerous.24
Matrix patches imbed the drug into the adhesive matrix. As the matrix breakdowns, it releases the drug slowly.22It is generally safe to cut these patches, as it does not affect the release mechanism.24
Patches are easy to apply. Select the application site based on package instructions, making sure the area is clean, dry, and relatively hair-free.
Remove the patch from packaging. Peel back the protective backing to reveal the adhesive. Without touching the adhesive, apply the patch to the desired area.
Press the patch firmly to the area and wear it no longer than the manufacturer's recommended time. When removing the patch, peel it gently away from the skin. Fold the patch in half so the adhesive backing is stuck to itself.
Discard the patch in a trash receptacle that is out of reach from pets and children, as there can be residual drug in the used patch.24
Epinephrine Auto-Injector
In 2009, 225 people died from anaphylactic reactions.26
The EpiPen auto-injector is used for life-threatening anaphylaxis. All patients and their caregivers should be taught how to use the EpiPen, and its practice pen makes teaching patients convenient and effective.
First, check the EpiPen’s expiration date and ensure the solution is clear. When an EpiPen is warranted, flip open the carrier cover and slide the pen out.
Grab the injector with the orange tip down, as this is where needle comes out. Remove the blue safety top.
Now, bring the orange tip to the outer thigh with moderate force (no need to remove clothing). The next steps are important and not intuitive.
Once it clicks, hold the pen there for 10 seconds. Massage the area for 10 seconds while calling 9-1-1. Bring the EpiPen to the emergency room.27
Naloxone Auto-Injector
In 2012, 9869 people died from painkiller overdoses, and additional 3665 from heroin overdoses.28
Evizo is a naloxone auto-injector approved for opioid overdose. This device uses visual and audio instructions to assist caregivers.
To use the device, remove the auto-injector from the outer case. Once it is ready to inject, remove the red safety cap.
Be careful not to touch the black base, as this is where the needle resides. Place the black end against the middle of the patient’s thigh (no need to remove clothing), press firmly on the top of the device, and hold the device in place for 5 seconds.
A click and hissing should be present, which means the device is working properly. After administration, get medical help. If symptoms return, use an additional Evzio device and repeat every 2 to 3 minutes as needed.29
Conclusion
Retail clinicians will see a plethora of delivery devices, each with its own directions for use in its package. Studies have demonstrated a need for better clinician education, as well as an increase in patient-clinician interactions.10
It’s best to show the patient how to use the device and have them teach it back. Simply providing written material or verbal instruction is largely ineffective.
References
- FDA. Frequently Asked Questions About Combination Products. Available at http://www.fda.gov/CombinationProducts/AboutCombinationProducts/ucm101496.htm. Accessed on December 1, 2015.
- Byron PR. Drug delivery devices: Issues in drug development.Proc Am Thorac Soc.2004;1:321-28
- Becker’s Hospital Review. 7 key statistics on retail clinics. Available at http://www.beckershospitalreview.com/hospital-physician-relationships/7-key-statistics-on-retail-clinics.html. Accessed November 18, 2015.
- Fierce Practice Management. The top 3 reasons patients visit retail clinics. Available at http://www.fiercepracticemanagement.com/story/top-3-reasons-patients-visit-retail-clinics/2015-05-13. Accessed November 18, 2015.
- American Medical News. Walgreens clinics expand services to diagnosing chronic diseases. Available at http://www.amednews.com/article/20130422/business/130429980/7/. Accessed on November 18, 2015.
- US Centers for Disease Control and Prevention. Asthma. Available at http://www.cdc.gov/nchs/fastats/asthma.htm. Accessed November 15, 2015.
- American Asthma Foundation. The Impact of Asthma. Available at http://www.americanasthmafoundation.org/impact-asthma. Accessed November 15, 2015.
- Geller DE. Comparing clinical features of the nebulizer, metered-dose inhaler, and dry powder inhaler.Respiratory Care.2005;50:1313-22.
- Hashmi A, Soomro JA, Memon a, et al. Incorrect inhaler technique compromising quality of life of asthmatic patients.J Medicine.2012;13:16-21(inadequate technique is leading cause of treatment failure)
- Bjermer L. The importance of continuity in inhaler device choice for asthma and chronic obstructive pulmonary disease.Respiration.2014;88:326-52
- American Academy of Allergy Asthma and Immunology. Inhaled Asthma Medications. Available at http://www.aaaai.org/conditions-and-treatments/library/at-a-glance/inhaled-asthma-medications.aspx. Accessed on November 19, 2015.
- Asthma Society of Candida. How to Use Your Inhaler. Available at http://www.asthma.ca/adults/treatment/meteredDoseInhaler.php. Accessed on November 17, 2015.
- Asthma Society of Candida. How to Use Your Inhaler. Available at http://www.asthma.ca/adults/treatment/spacers.php. Accessed on November 17, 2015.
- Asthma Society of Candida. How to Use Your Inhaler. Available at http://www.asthma.ca/adults/treatment/diskus.php. Accessed on November 17, 2015.
- Health for UK Healthcare Professionals. How to use the Ellipta Inhaler. Available at http://hcp.gsk.co.uk/therapy-areas/respiratory/patient-information/how-to-use-ellipta-demo-inhaler.html. Accessed November 10, 2015.
- American Diabetes Association. Fast facts data and statistics about diabetes. Available at http://professional.diabetes.org/admin/UserFiles/0%20-%20Sean/Documents/Fast_Facts_3-2015.pdf. Accessed on November 12, 2015.
- Diabetes Self-Management. Everything you ever wanted to know about injecting insulin. Available at http://www.diabetesselfmanagement.com/managing-diabetes/treatment-approaches/everything-you-ever-wanted-to-know-about-injecting-insulin/, Accessed November 10, 2015.
- LiveStrong. How to use insulin syringes and needles. Available at http://www.livestrong.com/article/324019-how-to-use-insulin-syringes-and-needles/. Accessed on November 12, 2015.
- Diabetic Living. How to use an insulin pen. Available at http://www.diabeticlivingonline.com/medication/insulin/how-to-use-insulin-pen?page=1. Accessed on November 12, 2015.
- Pfizer. User Sharps Disposal — Frequently Asked Questions (FAQs). Available at https://www.pfizer.com/files/responsibility/protecting_environment/Used-Sharps-Disposal-FAQ.pdf. Accessed on December 1, 2015.
- Afrezza. Inhaling Afrezza Insulin. Available at https://www.afrezza.com/step-by-step-guide. Accessed November 12, 2015.
- Walter JR, Xu S. Therapeutic transdermal drug innovation from 2000 to 2014: Current status and outlook. Drug Discov Today.2015;20(11):1293-9.
- Prausnitz MR, Langer R. Transdermal drug delivery.Nat Biotechnol.2008; 26(11): 1261—1268.
- PL Detail-Document. Characteristics of transdermal patches. Pharmacist’s Letter/Prescriber’s Letter. August 2012.
- Lexi-Comp, Inc. (Lexi-Drugs). Lexi-Comp, Inc.; January 29, 2015
- American Academy of Allergy Asthma and Immunology. Death from anaphylaxis is a reassuringly unusual outcome. Available at reactions http://www.aaaai.org/global/latest-research-summaries/Current-JACI-Research/death-anaphylaxis.aspx. Accessed on November 18, 2015.
- EpiPen. How to use your EpiPen (epinephrine Injection) Auto Injector. Available at https://www.epipen.com/en/about-epipen/how-to-use-epipen. Accessed on November 18, 2015.
- The Guardian. Fatal heroin overdoses double across much of US in two years. Available at http://www.theguardian.com/society/2014/oct/03/heroin-overdose-deaths-us-doubles-painkillers-addiction. Accessed November 18, 2015.
- Evizo. How to use EVIZO. Available at http://www.evzio.com/hcp/about-evzio/how-to-use-evzio.php. Accessed November 18, 2015.
