Appreciating the Big Picture of ICD-10
As the last country with a modern health care system to adopt ICD-10, the United States is finally hopping on the bandwagon just before the anticipated release of ICD-11 in 2018.
"Better late than never” should be the slogan for the United States transition to theInternational Classification of Diseases, 10th Edition(ICD-10). As the last country with a modern health care system to adopt ICD-10, we are finally hopping on the bandwagon just before the anticipated release of ICD-11 in 2018.
Although the transition from ICD-9 to ICD-10 may be bumpy, it presents an immense opportunity to improve population health and more efficiently allocate health care resources. The purpose of this article is to provide an overview of ICD-10, including its history, major differences from ICD-9, benefits, and implications for retail-based nurse practitioners.
What Is ICD-10?
Developed by theWorld Health Organization(WHO) in 1992, ICD-10 outlines a coding system that classifies diseases and other health problems in order to accurately store and retrieve diagnostic information. Precise coding enables analysis of epidemiological data, which can be used to paint a picture of the overall health of a specific geographic region or patient population. The ICD-10 records are used by WHO to compile national mortality and morbidity statistics, and individual countries use the information for reimbursement and resource allocation.
History of ICD-10
Work on this new diagnostic tool began back in 1983 whenReturn of the Jediwas blowing up the box office and every arcade reverberated with Michael Jackson’s “Billie Jean.” This was a time whenBack to the Futurewas still in the future and the concept of a personal computer with a mouse and user interface was yet to be invented. Yes, this was also before the Health Insurance Portability and Accountability Act, theMental Health Parity Act, and the first retail clinics.
From 1983 to 1992, experts worked tirelessly to revamp ICD-9. By 1994, ICD-10 was endorsed by the 43rd World Health Assembly and implemented by early adopters: Australia adopted ICD-10 in 1998, followed by Canada in 2000. Shortly thereafter, most European countries, as well as South Africa, Thailand, Korea, and China, followed suit. What happened to the United States, you ask?
The United States is the last developed country to adopt ICD-10. Complete Practice Resources1asserts that powerful, deleterious lobbyists caused this delay: “In the United States, where a complex health care system and highly influential special interest groups control decision making, it has made implementation difficult.”1In early 2009, the Department of Health and Human Services created an implementation date of October 1, 2013; however, bureaucratic red tape pushed this date to October 1, 2014,2and then to October 1, 2015.
So, here we are: more than 30 years after work on ICD-10 began, withStar Wars Episode VIIin development, Apple Watches on the scene, and the Affordable Care Act enacted, the United States has finally committed to implementing ICD-10. Today, 25 countries across the world also use ICD-10. Since its launch, however, ICD-10 has been subjected to an ongoing revision process and WHO anticipates thatICD-11will be released in 2018.
Big Changes in ICD-10
Not just a simple update, ICD-10 fundamentally changes the structure of coding to improve communication between health care stakeholders. The gravity of this change requires nurse practitioners to understand the importance of the transition, as well as the key differences between ICD-9 and ICD-10.
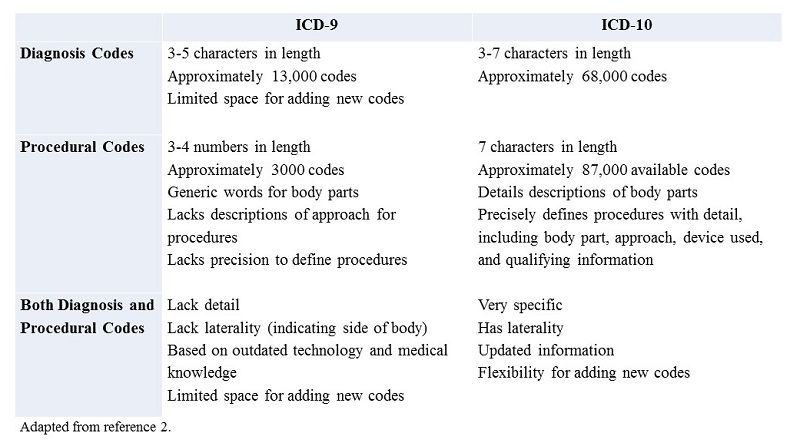
ICD-9 codes lack specificity. For example, if a child is seen for a burn on her left foot, the ICD-9 diagnostic code does not distinguish between the left or right foot. On the other hand, the ICD-10 codes specify the etiology, anatomic site, severity, and other clinical details, providing extra granularity. Many of the chapters within ICD-9 are full and inhibit the ability to add new codes. Moreover, terminology used in ICD-9 is outdated and does not reflect modern medical knowledge and technology.Table 12illustrates the main differences between ICD-9 and ICD-10 diagnosis and procedural codes.
Table 1: Comparison of ICD-9 and ICD-10 Codes
Benefits Across the Health Care System
The American Health Information Management Association (AHIMA) has been a long-time advocate for ICD-10 implementation. AHIMA summarizes the 3 key benefits of transitioning to this new and improved coding system, as follows: (1) greater specificity of data reporting, (2) increased coding accuracy, and (3) seamless reporting across international borders.
AHIMA asserts that ICD-10 will positively impact quality measurement, public health, organizational monitoring, health information technology (HIT), and reimbursement. In her article, “Why ICD-10 Is Worth the Trouble,” Sue Bowman, a registered health information administrator, succinctly and powerfully states, “Transitioning to ICD-10 is a major disruption that providers and payers may prefer to avoid. But it is an upgrade long overdue, and the benefits are far-reaching.”3
Quality Measurement
The biggest difference between ICD-9 and ICD-10 is the increase in specificity and granularity of diagnoses and procedures. This specificity elucidates the connection between the quality of care provided by the nurse practitioner and her patient’s condition. Complete and accurate codes also increase the quality of patient outcome data to ensure fair reimbursement.
Public Health
Sharing public health data across international borders is difficult when the United States continues to use outdated codes. The transition to ICD-10 encourages comparisons of global health data. WHO envisions that with widespread adoption of consistent ICD-10 documentation, every country will be able to detect and respond effectively to emerging disease threats.
Organizational Monitoring
The finer distinctions in diagnostic and procedural codes allow organizations such as payers, health care systems, and academic research centers to more accurately evaluate the effectiveness of new treatments. WHO also hopes that greater specificity will enable clinicians to evaluate their performance relative to other clinicians.
Health Information Technology
ICD-10 adoption will enable greater use of HIT. The robust and logical structure of ICD-10 translates easily into algorithms for modern software, including computer-assisted coding applications. These applications improve automatic code generation and data abstraction, natural language processing, work flow automation, management report generation, and system security.
Implications for Retail Clinics
Retail care staff will need to prepare for the ICD-9 to ICD-10 transition. Whereas most of the generic considerations apply across all health care settings, retail-based treatment presents with some unique challenges. For example, retail-based nurse practitioners may find it beneficial to brush up on the new ICD-10vaccinationandpreventive screeningcodes.
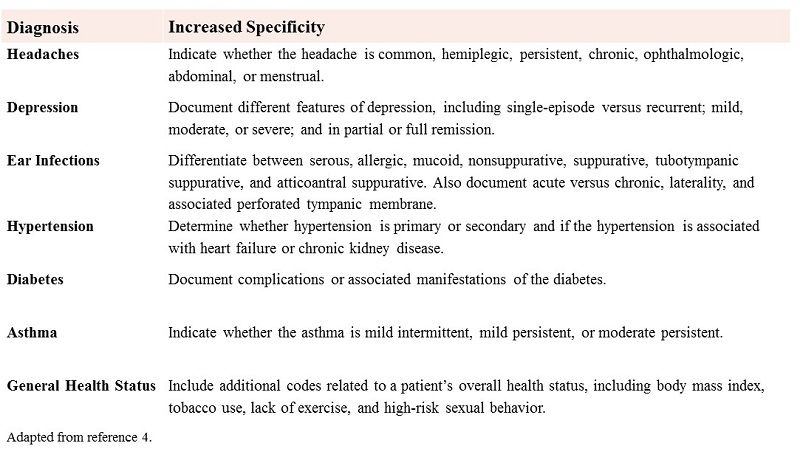
The biggest change in coding for retail clinics is the need for greater specificity. This requirement for more detail will be the most obvious across 7 diagnostic categories: headaches, depression, ear infections, hypertension, diabetes, asthma, and general health status (Table 24). Michelle Cavanaugh, a nurse and AHIMA-approved ICD-10 trainer elucidates these modifications in her article, “Seven Big ICD-10 Changes for Primary Care.4” For more information, the Centers for Medicare & Medicaid Services has developed resources specific to retail-based care patient presentations.
Table 2: Top ICD-10 Changes for Primary Care
Conclusion
This article presented a macro-level view of ICD-10, including its history, benefits, and implications for retail-based nurse practitioners. Despite its lack of punctuality, the United States health care system has begun adopting ICD-10. Although the transition from ICD-9 to ICD-10 will not be simple, the benefits to quality improvement, public health, information technology, and organizational management cannot be understated.
Dr. Melissa DeCapua is a board-certified psychiatric nurse practitioner who graduated from Vanderbilt University. She has a background in child and adolescent psychiatry, as well as psychosomatic medicine. Dr. DeCapua currently works as the Healthcare Strategist at a Seattle-based health information technology company where she guides product development by combining her clinical background and creative thinking. She is a strong advocate for empowering nurses, and she fiercely believes that nurses should play a pivotal role in shaping modern health care. For more about Dr. DeCapua, please visit www.melissadecapua.com or follow her on Twitter (@melissadecapua).
References
- The History of ICD-10. Complete Practice Resources website.www.cpticdpros.com/blog/the-history-of-icd-10/. Published September 5, 2012. Accessed September 30, 2015.
- American Medical Association. Preparing for the ICD-10 code set: October 1, 2014 compliance date. UnityPoint Health website.www.unitypoint.org/waterloo/filesimages/For%20Providers/ICD9-ICD10-Differences.pdf. Published September 25, 2012. Accessed September 30, 2015.
- Bowman S. Why ICD-10 is worth the trouble.J AHIMA. 2008;79(3):224-229:quiz 41-42.
- Cananaugh M. Seven big ICD-10 changes for primary care. Physicians Practice website.www.physicianspractice.com/icd-10/seven-big-icd-10-changes-primary-care. Published March 19, 2015. Accessed September 30, 2015.
